This fact box will help you to weigh the benefits and harms of early detection of breast cancer by mammography screening. The information and numbers are based on the best scientific evidence currently available.
This fact box was developed by the Harding Center for Risk Literacy.
Breast cancer develops when abnormal cells multiply in an uncontrolled manner and gradually turn into lumps or growths in the breast tissue. Cancer cells can infiltrate healthy tissue and metastasize (spread). Factors such as age, family history, and hormonal influences can affect the development of breast cancer. It is assumed that about 8 out of 100 cases of breast cancer are hereditary and can be traced back to the so-called “breast cancer genes” BRCA1 and BRCA2 [2].
Breast cancer is the most common cancer affecting women in Germany, with about 70,000 new cases each year [3].
Early detection (screening) targets people who do not show symptoms of a particular disease (here, breast cancer). The aim is to detect and treat breast cancer at an early stage in order to increase chances of recovery.
A mammography is an X-ray examination of the breast in which two X-rays are taken from different angles. These X-rays are each assessed independently by two doctors for signs of abnormalities that may be cancerous [4].
Women in Germany between 50 and 69 years of age can participate in mammography screening every two years. This service is paid for by German health insurance funds [5]. It is an organized screening program that women are personally invited by letter to attend.
Alternative early detection procedures include ultrasound (sonography) and magnetic resonance imaging (MRI) of the breast. It remains unclear whether these procedures help lower the risk of dying from breast cancer [4].
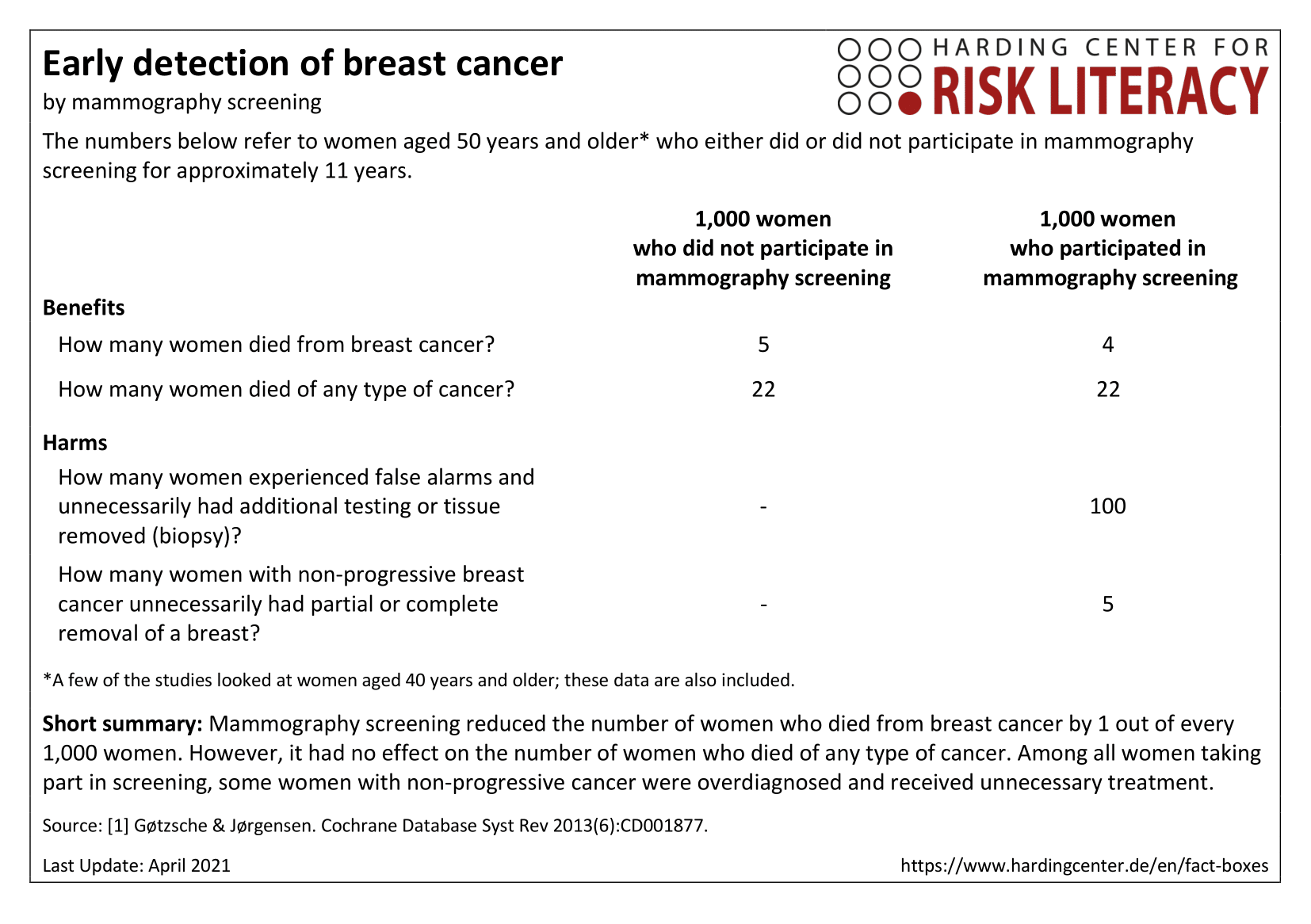
The fact box shows the benefits and harms of mammography screening compared to no mammography screening.
The table may be read as follows:
5 out of every 1,000 women aged 50 and over without screening and 4 out of every 1,000 women with screening died from breast cancer over a time period of approximately 11 years.
The numbers in the fact box are rounded. The numbers are calculated from eight studies that included a total of about 600,000 participants [1].
| Alter unter 50 Jahren | Alter von 50-74 Jahren | Alter ab 75 Jahren | Risikogruppen | |
| Frauen | - | X | - | - |
| Männer | - | - | - | - |
Erklärung der Symbole: X = für diese Personen gelten die Zahlen in der Faktenbox; (X) = auf diese Personen lassen sich die Zahlen unter Vorbehalt anwenden (in solchen Fällen ist eine Rücksprache mit ärztlichem Personal empfehlenswert); - = für diese Personen gelten die Zahlen nicht; ? = es ist unbekannt, ob die Zahlen für diese Personen gelten
On behalf of the Federal Joint Committee (a decision-making body of the joint self-government of physicians, dentists, hospitals, and health insurance funds in Germany), the German Institute for Quality and Efficiency in Health Care (IQWiG) developed an invitation letter and a decision aid for mammography screening [4].
The numbers in their decision aid differ slightly from those presented in the fact box. This decision aid presents data for women aged 50 to 69 who regularly participate in mammography screening for 20 years. Regularly participating in screening is said to save 2 to 6 out of every 1,000 women from dying from breast cancer [4].
Note, however, that most studies observed participants for about 11 years and that no study data are available for the time frame of 20 years [4]. Therefore, the numbers in the invitation letter are based on estimates only.
For that reason, the fact box shows numbers for women who participated in screening for approximately 11 years. It shows that regular participation can save 1 out of every 1,000 women from dying from breast cancer.
Screening did not affect the total number of deaths when all potential causes of death are considered. About 84 out of every 1,000 women died in total, independent of whether they were screened or not.
Furthermore, women who receive false alarms (positive test results that turn out to be false positives) can suffer from psychological distress, including anxiety and uncertainty, for years afterward [1].
A positive result from a mammography does not automatically mean that a woman has cancer. Mammography screening also detects preliminary stages of breast cancer, such as ductal carcinoma in situ (DCIS), which is characterized by abnormal cells in the mammary ducts that have not spread to other tissue (non-invasive). In some women DCIS remains harmless; in others it develops into an invasive tumor, which can be life-threatening [4].
Any screening can lead to overdiagnosis. In the case of breast cancer, this means that women are diagnosed with breast cancers that would have remained undetected without the screening. One instance of these are small tumors that grow slowly or not at all (non-progressive cancer) and might never have caused any complaints. Because it is difficult for physicians to assess whether a tumor will continue to grow, they often advise their patients to receive treatment.
Overdiagnosis often leads to overtreatment, which means unnecessary surgery or radiation [4].
Overall, the evidence is of moderate to high quality: Where the quality of evidence is moderate, further research is likely to have an important impact on some findings; where the quality of the evidence is high, the findings are very unlikely to be changed over the course of further research [6].
- April 2021 (update of the literature research, no new evidence)
- October 2019 (update of the accompanying text)
- April 2018 (update of the literature research, no new evidence; update of the accompanying text)
- November 2017 (creation)
Information within the fact box was obtained from the following sources:
[1] GøtzschePC, JørgensenKJ. Screening for breast cancer with mammography. Cochrane Database Syst Rev2013(6) doi: 10.1002/14651858.CD001877.pub5.
[2] Deutsches Krebsforschungszentrum. Krebsinformationsdienst. Familiärer Brust und Eierstockkrebs 2018. [https://www.krebsinformationsdienst.de/wegweiser/iblatt/iblatt-familiaerer-brust-u-eierstockkrebs.pdf?m=1516614027&] 01.10.2019.
[3] Robert Koch-Institut. Krebs in Deutschland 2011/2012 2015. [www.gekid.de/Doc/krebs_in_deutschland_2015.pdf] 27.09.2019.
[4] IQWiG. Einladungsschreiben und Entscheidungshilfe zum Mammographie-Screening 2014. [www.iqwig.de/de/projekte-ergebnisse/projekte/gesundheitsinformation/p14-03-einladungsschreiben-und-entscheidungshilfe-zum-mammographie-screening.6270.html] 15.09.2019.
[5] Gemeinsamer Bundesausschuss. Früherkennungsuntersuchungen im Überblick 2016 [www.g-ba.de/institution/themenschwerpunkte/frueherkennung/ueberblick/] 01.10.2019.
[6] Fitzpatrick-Lewis D, Hodgson N, CiliskaD, et al. Breast cancer screening 2011. [https://canadiantaskforce.ca/wp-content/uploads/2011/11/2011-breast-cancer-systematic-review-en.pdf] 01.10.2019.[6] Fitzpatrick-Lewis D, Hodgson N, Ciliska D, et al. Breast cancer screening 2011. [www.canadiantaskforce.ca/wp-content/uploads/2011/11/2011-breast-cancer-systematic-review-en.pdf] 06.12.2017.
Documentation on how the numbers in the fact box were determined is available on request.
