This fact box will help you to weigh the benefits and harms of oral contraceptives. The information and numbers are based on the best scientific evidence currently available.
The fact box was developed by the Harding Center for Risk Literacy.
Girls become fertile after their first menstrual period. This means that they can get pregnant when a sperm cell encounters a mature egg in a fallopian tube [1].
Contraception prevents an egg from being fertilized or implanted in the uterus and thus, hinders pregnancy. Nowadays, there are different hormonal and non-hormonal contraceptives. The most widespread are oral contraception pills (birth control pills) and the condom [1].
Combined oral contraceptives are a form of hormonal birth control. They contain two different types of hormones: estrogen and progestogen. Both are female sex hormones that influence the menstrual cycle. The amount of estrogen and progestogen in a birth control pill differs according to the brand of pill and the version of the pill (generation) it belongs to.
Oral contraception pills are taken for a 21- or 22-day cycle, followed by a break of six to seven days. During this break, menstruation takes place, but the contraceptive effect continues [1].
If taken daily and as instructed, the pill inhibits ovulation and eggs from maturing in the ovary. The hormones, estrogen and progestogen, thin the lining of the womb (endometrium) which makes it unlikely that an egg cell will be implanted, even if ovulation has taken place. Additionally, the mucus in the neck of the uterus that protects it from bacteria is thickened and becomes more difficult for sperm to penetrate [1].
Girls after their first menstrual period and women of reproductive age. Women who have diabetes, are overweight (with a Body-Mass-Index of over 25, which is calculated by dividing weight in kilograms by height and squaring the number [kg/m2]), or who are currently pregnant, breastfeeding, or who have recently had an abortion should not consider combined oral contraceptives.
Like other hormonal contraception methods, the combined oral contraceptive pill is available only by prescription. Prior to the age of 20, the costs are covered by German health insurance providers [1].
Other hormonal contraceptive methods include contraceptive skin patches or hormone-releasing contraceptive coils (IUDs or IUSs). Non-hormonal contraceptive methods include condoms or the natural birth control method (calendar method).
A decision about whether or not to use a contraceptive method depends on the reliability of the method, how it is tolerated and used, and on personal preferences and values.
Non-hormonal contraceptive methods have few or no side effects, but are less effective. The most widespread contraceptive method is the condom. If used correctly, the condom (also) provides protection from some sexually transmitted infections (STIs), such as the human immunodeficiency virus HIV, which can lead to AIDS [1].
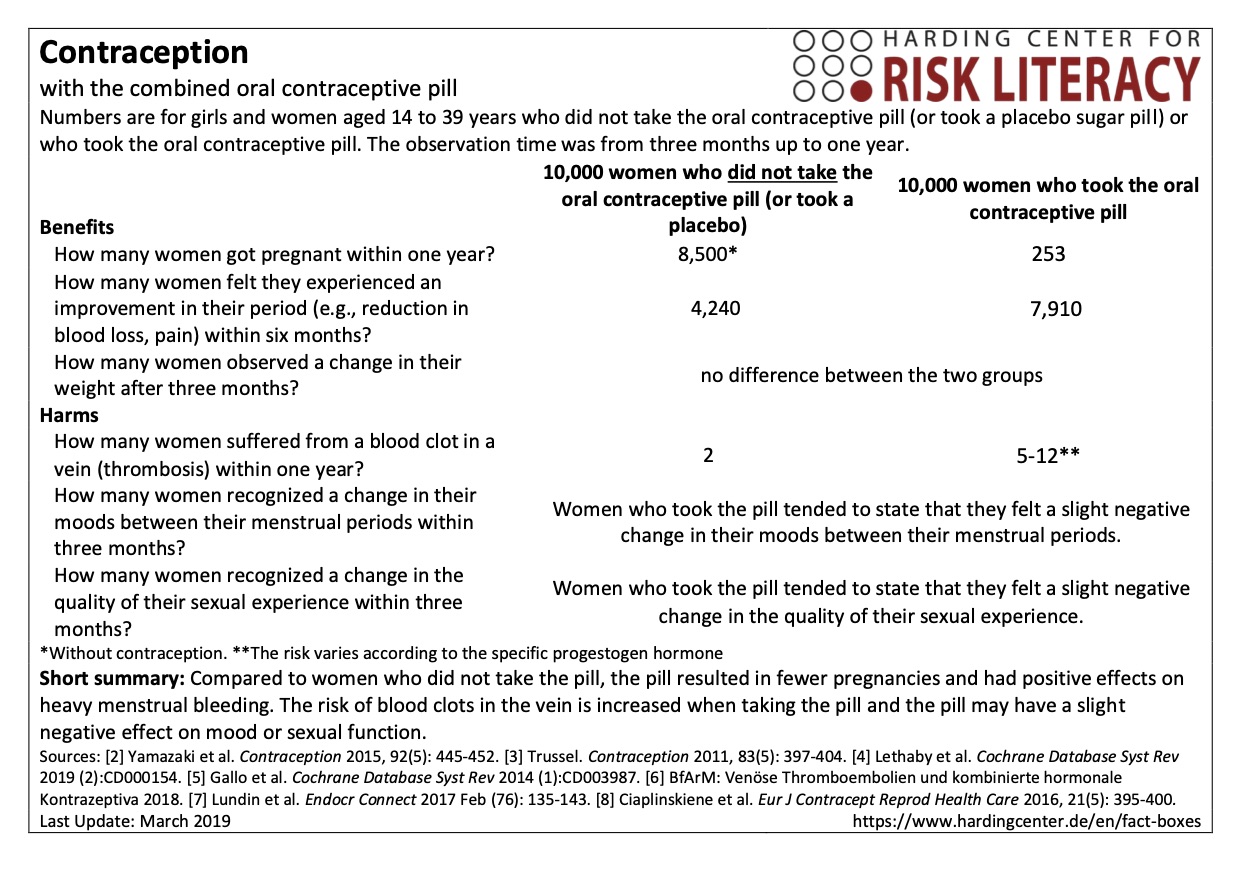
The fact box shows the benefits and harms of taking the oral contraceptive pill compared with a placebo or taking no pill.
The table may be read as follows:
Based on the results of the study, we can expect about 253 out of every 10,000 women will get pregnant within one year despite taking the contraceptive pill. Without using any contraception, we can expect about 8,500 out of 10,000 women will get pregnant within one year.
The numbers in the fact box are rounded.
Numbers for the benefits
The numbers on contraception when taking the pill are based on an analysis of seven studies on combined oral contraceptives with a total of around 14,000 participants. Each study is based on the Pearl index for typical use of the pill, which includes mistakes made while taking the pill (e.g. occasionally forgetting to take the pill). The Pearl index indicates the proportion of sexually active women who get pregnant within one year despite using any contraceptive. The following applies: the lower the Pearl index, the safer the contraceptive method. Information on the Pearl index with no contraceptive use is based on reviews of the reliability of contraceptives [2, 3].
The numbers for the influence of the oral contraceptive pill on the heaviness of menstrual bleeding are based on eight studies with about 800 participants [4].
The information on the influence of the oral contraceptive pill on body weight is based on three studies with about 200 participants [5].
Numbers for the harms
The numbers for the influence of the oral contraceptive pill on the risk of a blood clot in a vein (thrombosis) are based on an evaluation of all studies reported by pharmaceutical companies to the Federal Institute for Drugs and Medical Devices (BfArM), the European Medicines Agency (EMA) and other European authorities, summarized in 2013 and updated in 2018. The summary was prepared by the Federal Institute for Drugs and Medical Devices (BfArM) for German-speaking countries [6].
The information on the influence of the pill on mood perception is based on a study with about 200 participants [7].
The information on the influence of the pill on sexual desire is based on a study with 80 participants [8].
It should be considered that no contraceptive method is 100 percent safe. Safety depends, among other things, on correct and regular use. Forgetting to take the oral contraceptive pill will result in a decrease in reliability. Furthermore, the effectiveness of the oral contraceptive pill may be affected by obesity and under special circumstances, such as when the user experiences vomiting and diarrhea (e.g., food poisoning, stomach flu) [1].
In addition, taking the oral contraceptive pill at the same time as specific interacting drugs, such as seizure-preventing drugs (antiepileptics), antibiotics, mood-enhancing preparations (e.g. St. John's wort), the anti-nausea (antiemetic) medication “aprepitant” and the acne medication “isotretinoin” can influence the reliability of the pill [9].
The risk of a blood clot in a vein (thrombosis) differs across different types of oral contraceptive pills because they contain different progestogens. Pills containing the progestogens “levonorgestrel” or “norethisterone” and “norgestimate” (in first and second generation pills) have the lowest risk. About 5 to 7 thromboses per 10,000 women occur within one year [6].
About 8-11 out of 10,000 women taking the pill with the progestogen “dienogest” (in third and fourth generation pills) develop a blood clot within one year.
About 9-12 out of 10,000 women who take the pill with progestogens such as “drospirenone”, “gestoden” or “desogestrel” (in third and fourth generation pills) develop a blood clot within one year.
The risk of blood clot formation is unknown for progestogen-supplemented pills such as “chlormadinone” or “nomegestrol” (in third and fourth generation pills). Studies are planned or currently underway [6].
If a blood clot develops in a vein, usually in the deep veins in the leg or pelvis, the blood vessel can gradually become blocked. In this case, clinicians speak of thrombosis. If parts of the blood clot break loose, it is called an embolism. If an embolus enters the lungs, it can block the pulmonary vessels, resulting in cardiovascular failure, which in the worst case can be fatal (pulmonary embolism). Typical signs of deep vein thrombosis are severe pain in the leg, swelling of the leg, tension or heaviness in the leg and bluish-red discoloration and shiny skin on the leg. Typical symptoms of pulmonary embolism include: sudden difficulty breathing or shortness of breath, breath-dependent chest pain, tachycardia and unexplained cough (possibly with bloody sputum) [10].
In addition to the benefits and harms listed in the facts box, there are numerous studies that have investigated the long-term effect of the oral contraceptive pill on the risk of cancer. The results refer to women between the ages of 20 and 90 who either did or did not take the contraceptive pill.
Eight out of 19 studies showed that women who had taken the oral contraceptive pill at some point in their lives had a lower risk of developing colon cancer compared with women who never had taken the pill. Eleven out of 19 studies reported no differences between the two groups. It is not possible to estimate the number of women who did or did not develop colon cancer in each group. The results on the influence of the oral contraceptive pill on the risk of colon cancer could change with further research (moderate evidence) [12].
According to results of three studies, women who had ever taken the oral contraceptive pill appeared to have a lower risk of developing ovarian cancer than women who never had taken the pill. It is not possible to estimate the number of women who did or did not develop ovarian cancer in each group. The result on the long-term effect on ovarian cancer risk is not trustworthy (very low-quality evidence) [11].
Six out of 23 studies showed that women who had taken the oral contraceptive pill at some point in their lives had an increased risk of breast cancer compared with women who never had taken the pill. Three studies reported a reduction in breast cancer risk. Fourteen out of 23 studies found no difference between the groups. It is not possible to estimate the number of women who did or did not develop breast cancer in each group. The results on the influence of the oral contraceptive pill on breast cancer risk will very likely change with further research (low-quality evidence) [13].
A correlation between the risk of cervical cancer and pill intake could not be observed. The study results refer to 16 studies with about 15,600 participants. It is not possible to estimate the number of women who did or did not develop cervical cancer in each group. The results on the influence of the pill on the cervical cancer risk will very likely be changed by further research (low-quality evidence) [14].
Long-term effect on the risk of heart attacks and strokes
The results refer to women between the ages of 18 and 50 who either did or did not take the contraceptive pill.
Eight out of 24 studies showed that women who took the oral contraceptive pill at some point in their lives had an increased risk of suffering a heart attack or stroke compared with women who never took the pill. The risk of a heart attack or stroke increased as the dose of estrogen increased. Fifteen out of 24 studies found no difference, and one study showed a reduction in risk. It is not possible to estimate the number of women who did or did not suffer from a heart attack or stroke. The results on the influence of the pill on the risk of heart attacks and strokes will very likely be changed by further research (low-quality evidence) [15].
Overall, the evidence is of very low to moderate quality:
The evidence of the contraceptive reliability of the pill is of high quality. It is very unlikely that further research will change the results (high quality).
Further research may change the results on the effect of the pill on heavy menstrual bleeding, the risk of a blood clot (thrombosis) and mood change (moderate quality).
Further research will very likely change the results on the effect of the pill on weight change and sexual function (low quality).
- March 2019 (last update)
Authors
Christin Ellermann, Christoph Wilhelm, Julia Beckhaus
Information within the fact box was obtained from the following sources:
[1] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) (2017). Verhütung. Available from: https://www.informedhealth.org/contraception.2327.en.html
[2] Yamazaki, M., Dwyer, K., Sobhan, M. et al. (2015). Effect of obesity on the effectiveness of hormonal contraceptives: an individual participant data meta-analysis. Contraception, 92(5): 445-452.
[3] Trussell (2011). Contraceptive failure in the United States. Contraception, 83(5): 397-404.
[4] Lethaby, A., Wise, M. R., Weterings, M. A., et al. (2019). Combined hormonal contraceptives for heavy menstrual bleeding. Cochrane Database Syst Rev (2).
[5] Gallo MF, Lopez LM, Grimes DA, et al. (2014). Combination contraceptives: effects on weight. Cochrane Database Syst Rev (1).
[6] BfArM (Bundesinstitut für Arzneimittel und Medizinprodukte) (2018). Venöse Thromboembolien und kombinierte hormonale Kontrazeptiva. Available from: www.bfarm.de/DE/Arzneimittel/Pharmakovigilanz/KOK/_node.html
[7] Lundin C, Danielsson KG, Bixo M, et al. (2017). Combined oral contraceptive use is associated with both improvement and worsening of mood in the different phases of the treatment cycle—A double-blind, placebo-controlled randomized trial. Endocr Connect, 76: 135-43.
[8] Čiaplinskienė, L., Žilaitienė, B., Verkauskienė, R., et al. (2016). The effect of a drospirenone-containing combined oral contraceptive on female sexual function: a prospective randomised study. Eur J Contracept Reprod Health Care, 21(5): 395-400.
[9] Lupp (2016). Dtsch Arztebl International, 113(11), S.18.
[10] Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen (IQWiG) (2016). Was sind Blutgerinnsel und wie entstehen sie? Available from: https://www.informedhealth.org/what-are-blood-clots-and-what-causes-them.2238.en.html
[11] Cibula, D., Gompel, A., Mueck, A. O. et al. (2010). Hormonal contraception and risk of cancer. Human reproduction update, 16(6): 631-650.
[12] Luan, N.N., Wu, L., Gong T.T. et al. (2015). Nonlinear reduction in risk for colorectal cancer by oral contraceptive use: a meta-analysis of epidemiological studies. Cancer Causes Control 26: 65–78.
[13] Gierisch, J.M., Coeytaux, R.R., Urrutia R.P. et al. (2013). Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review. Cancer Epidemiol Biomarkers Prev., 22(11): 1931-43.
[14] Peng, Y., Wang, X., Feng, H. et al. (2017). Is oral contraceptive use associated with an increased risk of cervical cancer? An evidence-based meta-analysis. J Obstet Gynaecol Res. 43(5): 913-922.
[15] Roach, R.E., Helmerhorst, F.M., Lijfering, W.M. et al. (2015). Combined oral contraceptives: the risk of myocardial infarction and ischemic stroke. Cochrane Database Syst Rev (8).
Documentation on how the numbers in the fact box were determined is available on request.
